Key facts
Preventable and curable
At least one third of cancer cases could be prevented by limiting exposure to risk factors like tobacco, alcohol, and foods high in fats, sugar and salt. Another third could be cured if they were detected early and treated appropriately.
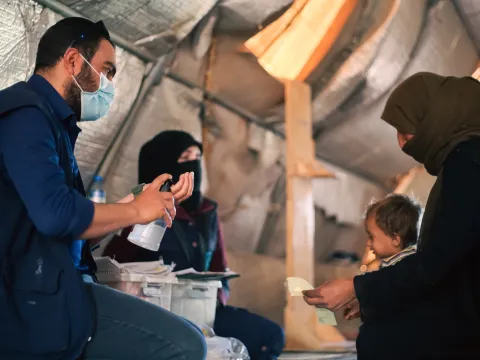
Driving inequity
Today, 70% of cancer deaths are happening in the least developed parts of the world. Even if you live in a higher income country, inequities still exist for lower-income, Indigenous, immigrant, refugee, rural, and other vulnerable communities.
The human and economic toll
Cancer takes a massive toll on households and families. While human suffering cannot be quantified with a price tag, the economic cost of cancer is estimated at US$1.2 trillion each year.